
Headway vs. Alma: Which is best for your practice?
Whether you’re a seasoned provider or just starting your practice, our analysis provides transparency so you can make the decision that works best for you.

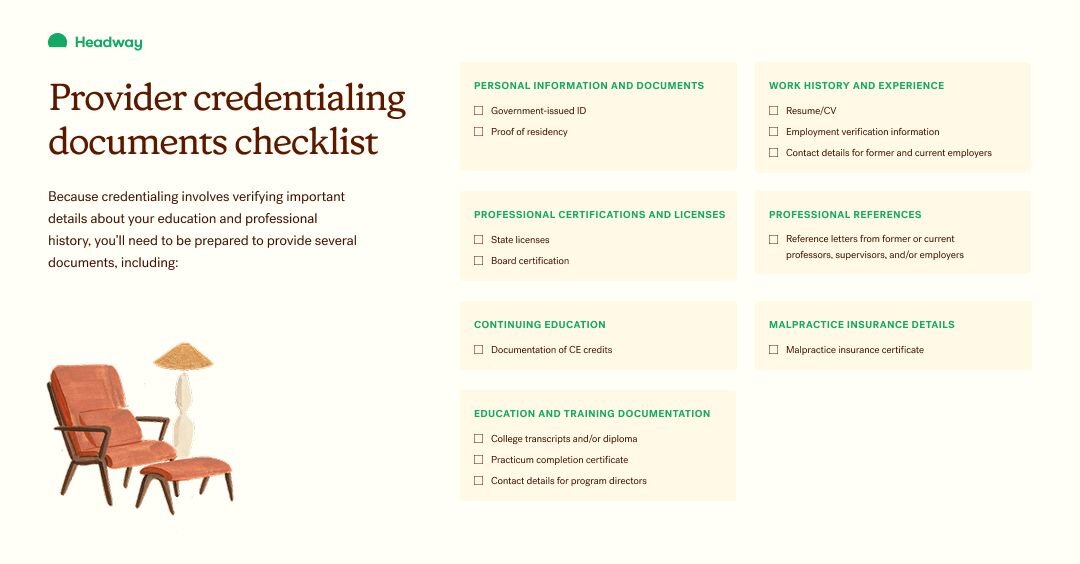
Because credentialing involves verifying important details about your education and professional history, you’ll need to provide several documents.
Billing insurance as a therapist is a great way to expand your practice — but the process of joining insurance panels can be complex and time-consuming. One important step, credentialing, involves providing a detailed background of your education and work experience to insurance payers. This process allows payers to confirm you’re qualified and compliant with important licensing and regulatory requirements.
There’s no way around credentialing if you’d like to join insurance networks, but you can take a few steps to make sure the process is as smooth and efficient as possible. Read on to learn more about provider credentialing and everything you need to do to bill insurance as a therapist.
Provider credentialing in mental healthcare refers to the process of verifying a mental health provider’s qualifications, professional history, and compliance with licensing and regulatory requirements in order to join an insurance panel.
While the process takes time, it’s important. It ensures providers meet important standards of care and are eligible to deliver services within a healthcare network or receive reimbursement from insurance payers.
CAQH, or the Council for Affordable Quality Healthcare, is a non-profit organization with the goal of streamlining the business of healthcare. Insurance plans use the information providers submit to CAQH to credential clinicians. The goal is to ensure all providers have the education, training, and experience to provide quality care to clients.
Mental healthcare providers can submit, maintain, and share information about their education and practice using an online database called CAQH ProView.
Credentialing mental health providers is important for a few reasons. First, the process ensures clinicians are qualified to provide mental health care by confirming they have the necessary education, training, and skills. Credentialing also ensures providers adhere to regulations that govern the mental health profession, along with ensuring ethical practice.
By promoting consistent standards for all in-network providers, these things ultimately promote safety for clients receiving care and protect insurance payers reimbursing therapists.
Mental health clinicians can practice with different education and licensing, including:
Because credentialing involves verifying important details about your education and professional history, you’ll need to be prepared to provide several documents, including:
Below, find our checklist as a downloadable PDF.
Headway makes it easy to get credentialed so you can begin seeing clients within 30 days. As an extension of your practice, Headway leverages the information you submit to CAQH to get you credentialed with all available plans at once, and with fewer errors and delays.
At Headway, we directly integrate CAQH into our onboarding process, using CAQH to pre-populate our intake form, so you can get started seeing clients through Headway as soon as possible. Our form also immediately flags any required information that might be missing from your CAQH account. Rather than being delayed by weeks, you can quickly adjust your intake form and move forward doing the work that matters most to you.

Whether you’re a seasoned provider or just starting your practice, our analysis provides transparency so you can make the decision that works best for you.

EHR systems can be costly. Looking for low-cost or free EHRs for mental health providers? Here are a few options and who they’re best suited for.

Learn more about the best options for mental health providers so you can make an informed decision for your practice.